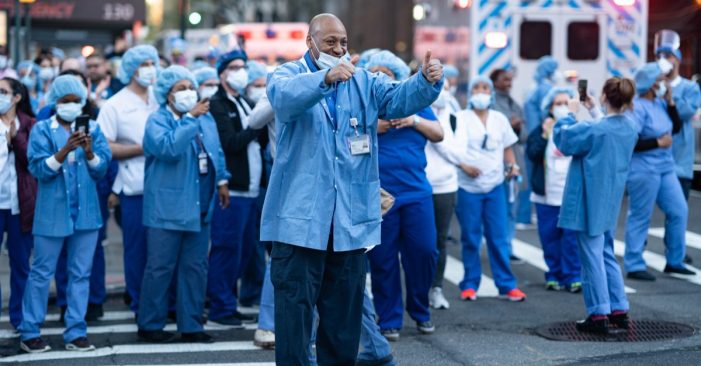
Nurses celebrate conquer of COVID-19 in New York City streets at 7 pm. New York City, New York / USA – April 19 2020 (Shutterstock)
By Linda N.
The month of April was a critical month for most New Yorkers, memories of frantic sounding sirens wailed down the almost empty streets, serving as evidence of the dire situation in New York as the virus ran rampage on and off the streets into homes and corners. Over eighty percent of issues covered in the news-media focused on the pandemic. It was tough, and the level of anxiety was very high. Fast track this scenario to June, and the narrative has changed significantly. There is a lull in an atmosphere that feels pregnant with hope and repressed energy, although tinged with a little bit of concern as the world awakens from forced slumber. The media has moved on to covering issues on recovery and the next steps post-COVID.
New York took a beating from the onslaught, exerting unimaginable pressure on everything – people and systems alike. One of the notable system worse hit during the period was the healthcare sector: Patients, family members, health workers, clinics, and hospitals; with daily heart-wrenching decisions on saving lives from a place of inadequacy ranging from medical supplies, testing materials, instruments, and personnel. Some resulted in the high number of deaths attributed to extraneous factors like inequalities borne from institutional injustice in the country, sector, and communities. The skewed nature of healthcare delivery revealed the massive gaps in the industry with the potential of having a lasting effect on the patients, the community, and health care providers. While the pandemic brought to the fore existing challenges post-COVID 19, it presents an opportunity to address and rectify some of the issues, before the next round of outbreak, which experts say will happen, later in the year.
Next steps for the New York State Health Care Post COVID-19
In a webcast panel discussion, organized by Crain’s New York Business on June 16, a set of New York healthcare experts discussed life after COVID-19, the changing impact of the pandemic on healthcare in the tri-state area.
Fred P. Gabriel, the Publisher/Executive Editor, Crain’s New York Business, moderated the online session with five healthcare experts. While delivering the opening keynote, Dr. Oxiris Barbot, MD Commissioner, New York City Department of Health and Mental Hygiene talked about the tracking and importance of public health indicators. The Commissioner said that “over 200,000 New Yorkers were diagnosed with COVID-19, and 21,000 individuals died as a result of the virus.” Figures touted by the media over the past couple of weeks. She also confirmed that the pandemic disproportionately affected Hispanics/Latinos and Blacks and Brown New Yorkers. She explained that patients from these ethnic groups died at twice the rate of whites in New York. According to her, “confirmed the long-standing racial disparities which are attributable to structural racism. Besides, the pandemic revealed the lapses within the structures, especially the absence of coordination between the state health care system and the primary healthcare providers who operate within the communities.”
She further explained that the pandemic revealed a lot of health care disparities, especially with primary care. They were not factored into the management plan equation; thus, they were not provided the required financial support needed to operate, explicitly promoting payment regulations around telemedicine, accessing personal protective equipment, and general support. As a result, major hospitals became overwhelmed during the pandemic.
Despite all these challenges, the Commissioner said, they were able to manage the situation through technology, especially multilingual technology. They conducted town halls and run campaigns to raise awareness, engage social service partners, and use direct mailing and robocalls to reach community members. This approach made up the equity action plan that maximized opportunities for the underserved, underrepresented community members to access the health care support needed.
Post COVID-19, it is evident that health care cannot return to ‘business as usual.’ There are several strategies being implemented in response to the new ‘normal’ of health care delivery and management. According to the Commissioner, these approaches entail “rethinking the system with an emphasis on exploring ways to help people gain access to care in a different way that will keep them safe, while simultaneously addressing issues of health and equity alongside linguistic and cultural differences.”
To reiterate some of the issues mentioned, Dr. Jacqueline Delmont, Chief Medical Officer, SOMOS Innovation LLC, emphasized the role of technology moving forward. As a practitioner, she claimed that using portals for communication, employing user-friendly support, and creating awareness of the new way of health care management and support are suggestions for the new face of health care delivery after the pandemic. However, she also raised similar concerns over the payment of this new way of providing services and delivery- support. One of the matters included how to ensure that telemedicine payment becomes a permanent approach considered by the health care management and stakeholders and that access to people who can provide support for the new telemedicine model needs to be resolved.
Addressing the issue of Primary Care Support in New York, Louise Cohen, Chief Executive Officer, Primary Care Development Corporation, noted that primary care in the post COVID era needs a new perspective towards global payment. Secondly, an immediate change in the New York State regulatory environment, which proved that it could be fast-moving as seen during the pandemic, is required, especially as “practitioners need capital to renovate, update and make them appropriate to operate.” Additional suggestions from Dr. Adam Reed Stracher, Chief Medical Officer and Director of the Primary Care Division, Weill Cornell Physician Organization, stressed sustained changes that need to occur in a spectrum. These changes ranged from payment for telemedicine, phone-calls, improved payment systems, and providing grants for implementation as suggestions for success during the period.
Noting the impact of regulatory issues towards the successful execution of a better healthcare service, some of the recommendations made include the need to repair the public health infrastructure deliberately. Also, developing the right model towards managing home care services and improving behavioral health, particularly, identifying how to treat patients without exposing them to the dangers of contracting COVID -19.
Conclusively, health care management, and delivery post-COVID-19 is changing. Telemedicine is the new normal that will drive operations, “because it meets people where they are, leveling the playing field and removes the barrier of traveling.” However, the experts, especially the practitioners, quickly mentioned that it does not deliver all aspects of care management. Still, it reduces the amount of time that the patient will spend in the medical facilities (except patients that require hospitalization and physical contact) and lessens risk.
Ultimately, there is a need to balance telemedicine and in-person health delivery. Some of the next steps towards this include providing financial support to the primary care practitioners, increasing access to technical support for upgrading to the new way of operation, supporting patients with reliable monitoring tools, and adequate training, especially those with long term health conditions. A combination of patient-driven health care, reformed payment regulatory policies, upgraded technology, increased awareness, behavior change communication, and newly skilled personnel will ensure that the health care sector is well prepared to address the fallout of COVID-19 and in the future.